Traumatic brain injury is a substantial head injury that results in damage to the brain. This damage can cause a wide spectrum of possible health outcomes.
Traumatic brain injury (TBI), also known as intracranial injury, is a substantial head injury that results in damage to the brain. This damage can cause a wide spectrum of possible health outcomes. Factors that are likely to influence neuropsychiatric outcome in TBI can be classified as pre-injury, injury and post-injury factors.
Injury-related factors include a) the type of physical injury and b) the vulnerability of certain brain areas to physical injury more than others. Biomechanical forces include inertial forces such as translation, rotation and angular momentum come into play, which can result in shearing of white

matter, contrecoup injury (e.g., boxing). Blast-related (explosive) injury is due to shock waves in open environments or complex wave forms in closed areas, which is furthered by secondary factors such as impact and penetration of bomb fragments and debris and tertiary factors including displacement of the whole body or body parts (acceleration) and subsequent deceleration and impact on obstacles. Quaternary effects of blast-related injury include body rupture at contact range of charge, burns from the explosion fireball, hot gases and induced fires, respiratory obstruction from toxic gases and dust, structural collapse, vagally mediated “pulmonary defensive reflex” and psychological stress.
Certain cortical areas and white matter projections are highly vulnerable to TBI. White matter injuries can be classified as primary axotomy, or cutting by sharp, penetrating objects or traumatic axonopathy, resulting from shearing caused by inertial forces. White matter tracts that run vertically (from the head to the feet) running axons in the brainstem, ventral forebrain, septo-hippocampal pathway and in anterior and midline cerebral areas are more vulnerable to injury. Frontal and temporal grey matter is more vulnerable than other grey matter regions to contusion injuries, due to the sharp edges and protrusions in the anterior and middle cranial fossae in the skull. Severe focal shearing injury can lead to tearing of fragile venous sinuses, haemorrhage and the formation of porencephalic cysts.
Biomechanical injury to neurons elicits stretch-induced action potentials, which result in ‘acute neurotransmitter storms’, i.e., increases in glutamate, dopamine, norepinephrine, serotonin and acetylcholine, which are potentially neurotoxic and functionally disruptive. The mechanism underlying neurotoxicity is increased intracellular calcium (Ca2+), which triggers a cascade of events including protein activation, mitochondrial dysfunction and free radical production, culminating in cell death. Survival of TBI seems to be related to normalization of these neurotransmitter levels in the days to weeks following TBI. Cerebral cholinergic nuclei in the basal forebrain leading to loss of cholinergic afferents and dysfunction of acetylcholine dependent circuits may underlie cognitive deficits in TBI. Chronic primary or secondary dysfunction in serotonergic, dopaminergic and norepinephrinergic neurons and and their target circuits may underlie neuropsychiatric consequences of TBI.
Uncoupling of cerebral blood flow (CBF) and glucose metabolism is another consequence of biomechanical injury. Experimental models of fluid percussion injury have shown that CBF may be reduced by 50%. Furthermore, hyper glycolysis due to neuronal activity following stretch-induced injury then leads to mismatch between energy supply and demand and neuronal dysfunction and/or death. The CBF-glucose metabolism mismatch may complicate the interpretation of functional imaging techniques that are predicated on the normal relationship between CBF and glucose metabolism.
Regional vulnerability to TBI also results in specific behavioural manifestations. Changes in emotional processing and social cognition have been associated with orbitofrontal cortex damage, in executive functions, i.e., attention, memory retrieval, judgment, decision-making with dorsolateral prefrontal damage, in learning, memory encoding and semantic aspects of language with temporal cortex damage, in emotional learning and responsiveness with amygdala damage, in declarative memory with entorhinal-hippocampal damage and in processing speed with white matter damage.
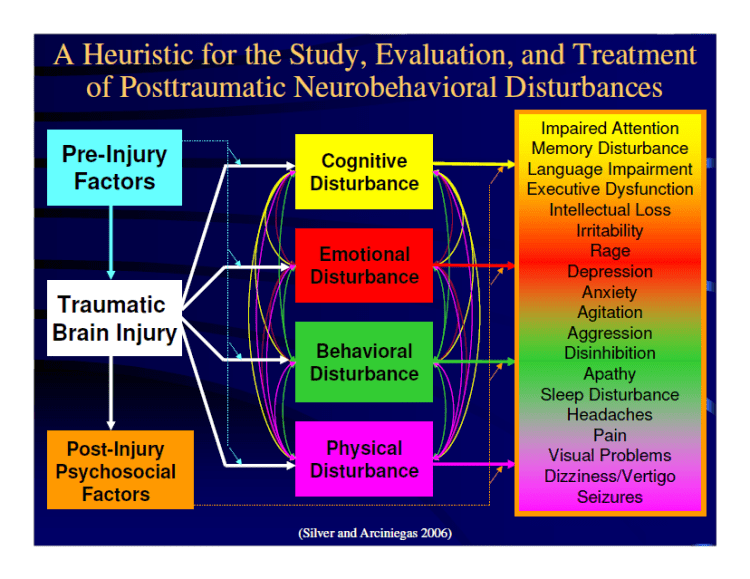
Pre-Injury Factors Influencing Neuropsychiatric Outcomes Of TBI:
- Age & gender: TBI is the leading cause of death in young male adults
- Lower baseline intellectual function is associated with worse outcome
- Pre-injury presence of one or more Axis 1 psychiatric disorders increases the incidence of post-TBI psychiatric manifestations; e.g., major depression prior to TBI has a three-fold increase following TBI
- Pre-injury sociopathy, risk-taking, novelty-seeking behaviour and aggression can lead to a greater risk of TBI and are associated with worse outcomes.
- Genetic factors that can influence cognitive and behavioural outcomes of TBI include those whose products affect neuronal plasticity (ApoE and BDNF), those that influence neuronal metabolism (COMT, DRDR, TAQ1, ANKK1) and genes that confer risk for adverse neurological outcomes (TDP43).
Post-Injury Factors Influencing Neuropsychiatric Outcomes Of TBI:
- Untoward medical complications
- Failure to receive medical, neurological, psychiatric or neurorehabilitative interventions in the early post-injury period, which is very important for improved functional outcomes
- Lack of education regarding the course of recovery and interpretation of symptoms.
- Lack of family, friends or resources to support recovery
- Premature return to work/school with ensuing failure to perform at expected levels
- Poor adjustment to or coping with disability by injured person or family.
- Litigation or other legal entanglements.
Studies indicates that the disabilities most often associated with TBI include cognitive, emotional, and to a lesser extent – sensory and motor impairments. A traumatic brain injury may permanently alter a person’s career or vocational aspirations and may also have profound effects on social and family relationships. In part, impairment of cognitive function may result in the loss of communication skills and memory, inability to organize tasks and solve problems, and decreased attention to detail.
In conclusion, an effective public health response to TBI also requires concerted programs to minimize adverse outcomes among persons who do experience injury. We need research activities to improve the acute care and rehabilitation of persons with TBI, strategies to ensure they have access to appropriate care and services, and interventions to promote their independence and integration into the community for persons living with the effects of TBI.
To help persons living with the effects of TBI, we need better information on the nature and scope of these disabilities, including who experiences TBIs, which rehabilitation treatment methods are most effective, and what services are useful and readily available.
Further Reading: Understanding Traumatic Brain Injury
Arciniegas DB, Anderson CA, Topkoff J, & McAllister TW (2005). Mild traumatic brain injury: a neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatric disease and treatment, 1 (4), 311-27 PMID: 18568112
Bigler ED (2001). Distinguished Neuropsychologist Award Lecture 1999. The lesion(s) in traumatic brain injury: implications for clinical neuropsychology. Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists, 16 (2), 95-131 PMID: 14590180
Bigler ED (2007). Anterior and middle cranial fossa in traumatic brain injury: relevant neuroanatomy and neuropathology in the study of neuropsychological outcome. Neuropsychology, 21 (5), 515-31 PMID: 17784800
Great article. I know treatments for these types of injuries are constantly being researched and in different stages of development. As you mentioned that brain stimulation goes back to the increase in intracellular calcium, so why not go to the source of the problem? There’s different techniques which have been tested on lab animals as far as blocking glutamate synapses or blocking calcium entry and they have shown benefits but not yet on humans (Minnerup, Sutherland, Buchan, & Kleinschnitz, 2012). Perhaps if this were researched further and better forms of treatment regarding controlling the calcium were developed, it could have a major impact on TBI treatment. I also read about how controlling overstimulation can be done so by cooling the brain, specifically in instances like stroke (Yenari & Han, 2012). I’m curious if cooling is also used in instances on TBI and what the long term outcome is like when cooling is used.
Research has been done showing that cannabinoids have been used on stroke patients to minimize the damage (Schomacher, Muller, Sommer, Schwab, & Schabitz, 2008). Perhaps there could there be some type of cannabis based medication that could be given along with the cooling that could minimize the damage until the patient becomes stable.
As you mentioned in the ending, a better understanding is needed to help patients who suffer from a TBI. If the damage can’t be controlled in the short term, more research is needed as far as rehabilitation to help give these patients back what they’ve lost.
– Daniel M.
This is a well written informative article. As mentioned, is quite difficult to help those recovering from brain injuries such as these. Although the brain does it’s best to preserve itself, an injury of this magnitude causes problems long after the wounds have healed. After the initial injury, neurons are disrupted which results in depolarization and a release of excitatory neurotransmitters. This releases Ca and Na ions which may lead to cellular breakdowns. Another aspect we wish to avoid is the breakdown of the blood brain barrier. There can be direct injury to the barrier in the primary phase and in injury to the endothelium of it in the secondary phase. This increases permeability of the blood vessels and can even lead to cell death. Of course there are theories that brain reorganization may be an answer to this type of brain injuries. Some research indicates that learned non-use of a paretic limb, combined with an increased reliance on the unaffected limb can result in major brain reorganization. This would be beneficial to a stroke patient. It is my hope that in the future we can find more ways to improve the quality of life of those with severe brain injury.